One in 20 people in Canada skip doses or prescriptions due to cost
This new research surveyed more than 223,000 Canadians ages 12 and older, and found that five per cent of respondents skipped prescribed medications due to cost.

Photo credit: Bacho Foto on Adobe Stock.
High costs keep one in 20 Canadians from being able to take their medications as prescribed, highlighting critical gaps in Canada’s healthcare system, according to new research from UBC published in the Canadian Medical Association Journal.
In a nationally representative study of more than 223,000 Canadians ages 12 and older, researchers found that five per cent of respondents skipped doses, delayed refills or didn’t fill prescriptions at all due to out-of-pocket costs. Women were 44-per-cent more likely than men to report such cost-related nonadherence. Rates were disproportionately high among gay or lesbian individuals, who were 16-per-cent more likely than their heterosexual counterparts to skip medications. Similarly, bisexual, pansexual and questioning individuals were 25-per-cent more likely to forgo their medications.
“Affordability challenges in Canada don’t stop at groceries—they extend to vital medications. This study sheds light on how personal, health and systemic factors intersect to affect prescription adherence,” said senior author Dr. Mary De Vera, associate professor at UBC’s faculty of pharmaceutical sciences.
Females, for example, are more likely to skip or reduce their medications due to competing priorities such as balancing caregiving, work and personal health. Dr. De Vera also notes that financial challenges, exacerbated by females generally earning less than males, contribute to their increased likelihood of cost-related nonadherence.
Vulnerable groups and geographic disparities
Young adults aged 18–34 were nine times more likely than those aged 75 or older to report cost-related nonadherence. Racial and ethnic minorities, including Indigenous, Latin American and Black communities, had 20- to 67-per-cent higher odds than White individuals of skipping or reducing medication due to cost.
Geographic disparities also emerged. Residents of Quebec, which has one of Canada’s most robust provincial drug insurance programs, were least affected by prescription costs. In contrast, inconsistent public drug coverage across provinces, shaped by variations in eligibility, premiums and co-payment policies, leaves many Canadians dependent on private insurance or out-of-pocket payments.
Policy implications
The study, supported by five cycles of the Canadian Community Health Survey (2015–2020), offers the most comprehensive look to date at the factors influencing cost-related nonadherence. It builds on earlier research by study co-author and UBC professor Dr. Michael Law by analyzing a larger dataset over multiple years.
The findings come as Canada takes steps toward national pharmacare with the passage of Bill C-64 in October 2024. However, researchers caution that significant gaps remain and Canadians need certainty about when universal access to prescription drugs will become a reality.
“As policymakers work toward implementing pharmacare, we hope our findings will inform public drug coverage plans and reduce cost barriers. This is especially urgent as financial and demographic pressures continue to challenge Canada’s healthcare system,” said lead author Dr. Nevena Rebić, who conducted the analysis as part of her PhD work at UBC.

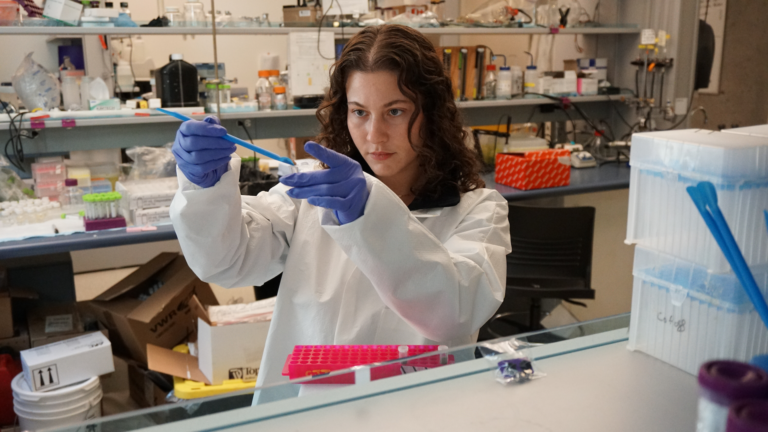
Featured Researcher
Associate Professor, Collaboration for Outcomes Research and Evaluation