Powerful, double-decker bus-sized microscopes help scientists uncover possible COVID-19 treatment
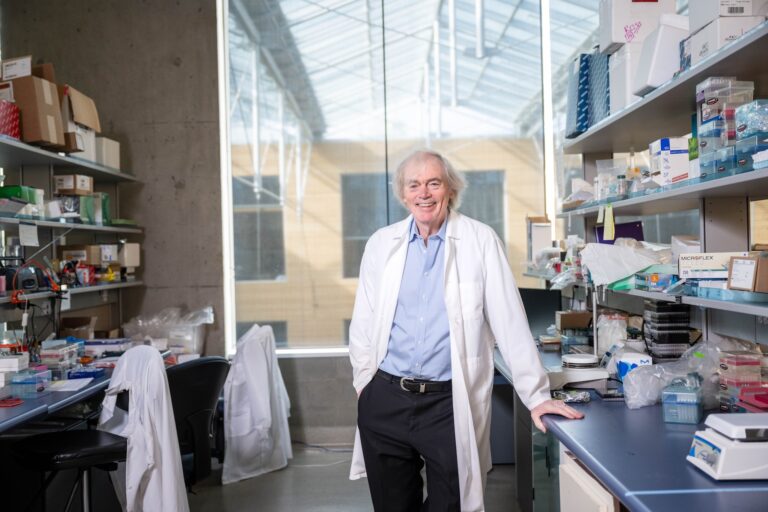
Researchers at UBC’s faculty of medicine are working with microscopes—some up to 13 feet tall—to help prevent and treat COVID-19.

The microscopes measure up to 13 feet in height, as tall as a double decker bus.
Researchers at UBC’s faculty of medicine are working with microscopes—some up to 13 feet tall—to help prevent and treat COVID-19.
The research team, led by Sriram Subramaniam, a professor in UBC’s department of biochemistry and molecular biology, is using a powerful imaging technique known as cryo-electron microscopy to take pictures at near-atomic resolution to see how various antibody treatments bind to the virus.
Their hope is to identify critical differences between antibodies that bind and block viral infection, and those that bind but are unable to block infection, providing powerful blueprints for drug and vaccine design. Already, they have helped to uncover how one antibody-based drug, known as Ab8, prevents and neutralizes the virus—a finding recently published in Cell.
How does cryo-electron microscopy work?
The SARS-CoV-2 virus is a hundred thousand times smaller than the size of a pinhead, making it undetectable using a regular light microscope. The proteins on the surface of a virus are even smaller.
To visualize the detailed shapes of viruses and proteins, we use cryo-electron microscopes. This powerful imaging technology uses beams of electrons to visualize shapes of tissues and cells using ultra-cooling, or “cryo” techniques—essentially, the imaging of samples at liquid nitrogen temperatures.
What exactly do your snapshots capture?
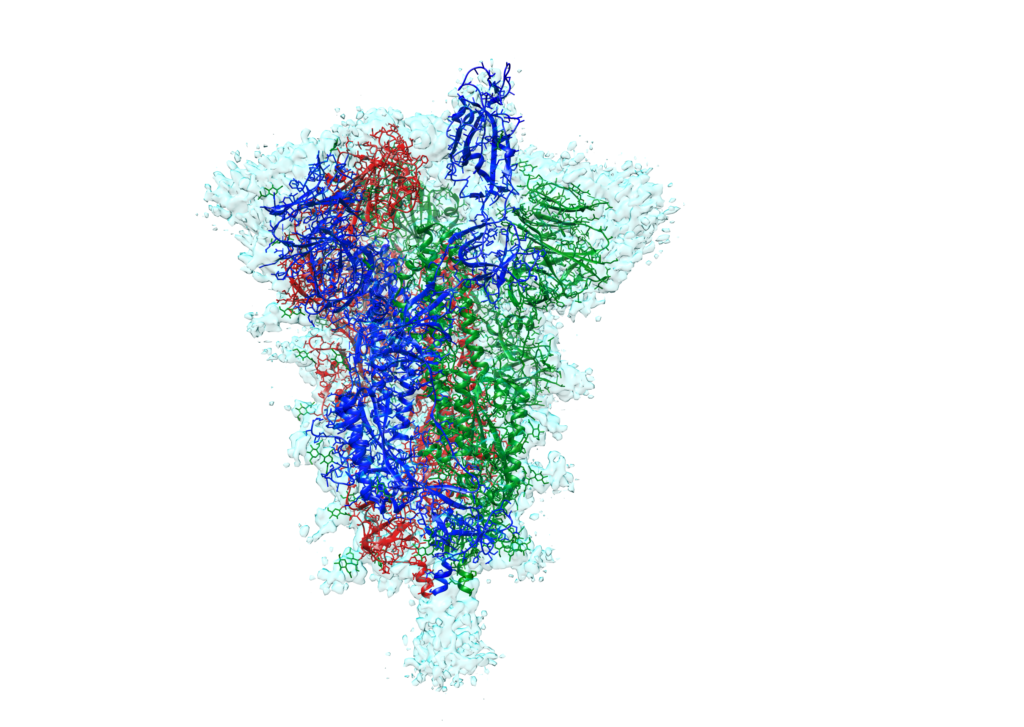
We’re generating structural images of the viral spike protein, which enables the coronavirus to enter human cells. Ultimately, using these microscopy pictures, we’ll be able to better understand the “hotspots” on the spike protein and provide information on how to improve the potency of treatments.
In our lab at UBC, we are able to determine the structures of proteins, such as the viral spike, at atomic detail in less than a day, providing powerful blueprints for drug and vaccine design.
For example, cryo-electron microscopy might be used in evaluating immune responses elicited by early vaccine candidates by characterizing how they bind to the spike protein. The antibodies may also be used as therapeutics themselves in patients actively suffering from COVID-19.
Why is it important to develop antibody-based therapies to treat COVID-19?
Most experts estimate it could take almost a year before there’s a vaccine that is effective and widely available. In the meantime, there’s an urgent need for antibody-based therapies to stem the progression and spread of COVID-19.
Understanding how these antibodies bind, and neutralize the virus, is crucial because it can be used by researchers who are developing treatments to understand and ultimately reduce drug-related side effects.
This is not just a critical element for treatment though. Knowing which types of antibodies provide protection against virus spread—and which ones are ineffective—will be essential in the evaluation of antibodies produced in vaccine trials.
You recently helped to uncover how one antibody-based drug, known as Ab8, prevents and neutralizes the virus. What is the significance of this finding?
Working with a team of scientists from the U.S., we employed our electron microscopy and advanced computing infrastructure at UBC to help evaluate and understand how this particular drug—constructed from an antibody component 10 times smaller than a full-sized antibody—neutralizes the virus in animal models. We have similar information emerging from our studies with other antibodies. Our expectation is that we will be able to use the structural information we derive about the precise footprints of antibody binding to develop more effective ways to stop SARS-CoV-2 in its tracks.
This particular finding has potential implications for both the prevention and treatment of COVID-19. The drug’s tiny size not only increases its potential for diffusion in tissues to better neutralize the virus, but also makes it possible to administer by alternative routes—including inhalation. Importantly, it only binds to the virus, leaving human cells untouched, which is a good sign that it won’t have negative side effects in people.
This research was supported by the Canada Excellence Research Chair Program, Genome BC, as well as a philanthropic gift made by an anonymous donor to VGH & UBC Hospital Foundation.